FULL SPEED AHEAD FOR VITAMIN D ..or precaution?
Vitamin D's popularity has soared to record heights. Bones, cancers, autoimmune conditions, diabetes, depression. You name it and there is most likely a vitamin D connection. With this new found popularity comes an array of higher and higher dosage products to satisfy the feeding frenzy. Reference 
UPDATE: This just un-covered. The body's activation of the hormone vitamin D form, the one that does most of the work, is influenced by slight variations in pH, or the acid alkaline balance. Even when body conditions, such as low calcium in blood and increasing PTH levels are indicating the hormone form of vitamin D should be activated, a slightly acid blood will suppress this action while a slightly alkaline level will increase. Mainly from animal studies and small human trials, needs immediate large scale human research NOW. Remember, the typical American diet is usually slightly acidic. This may be another reason to explain why vegetables and fruits along with weight-bearing exercise are the only two factors consistently showing value in maintaining bone strength. ---
- Is all the excitement justified?
This is an EXTREMELY CRITICAL issue today. Generally, a deficiency of vitamin D might exist thanks to skin cancer concerns and the avoidance of sun. The benefits of proper D levels are many and not just for calcium metabolism, but it is also linked with disease prevention, i.e. infections, cancers, depression, type 2 diabetes, and autoimmune conditions. Unfortunately, the story is missing one vital piece of the puzzle; LITTLE LONG TERM RESEARCH is available on the effects of these higher dosages now available. Many nutritionists are recommending these higher dosages based on the potential value, hoping that long term research will validate and no detrimental effects will show up. At least the toxicity level for vitamin D appears to be quite low until much larger amounts are consumed (20,000- 40,000 over time). But, vitamin D appears to be diphasic, meaning it has both low and high adverse effects. Determining any possible negative effects from these new higher dosages should be priority one, (2500+ IUs), until waiting for them to show up later.
- That is a large jump from the 400 IUs currently recommended**(see bottom of page for important update). How do these large amounts influence vitamin D blood levels? And how could such a wide difference develop?
First some general info. There are two forms of vitamin D circulating in the blood. A low activity form (passive D) and a high active form (hormone D). The vitamin D you supplement and the one that is produced from sunshine on skin modifying cholesterol, is processed in the liver and sent into the blood in the passive D form (25 OHD). This form serves as a storage material for the kidneys to use in making the high active D form (1,25OH2-D3), a hormone rather than a vitamin.
CAUTION: This is the conclusion from one of the referenced studies in this article: Both high and low concentrations of plasma 25(OH)D are associated with elevated risks of overall and cancer mortality. Low concentrations are associated with increased cardiovascular mortality. Now, before the explanation leading to this caution, here is how vitamin D functions.
FUNCTION OF VITAMIN D
The chief function of Vitamin D is in controlling calcium absorption and utilization into building strong bones. It is now known that this is a very narrow view of Vitamin D's many activities. To show how difficult vitamin D is to understand, here is a study of children with Rickets. Scientists predicted they would find the long held major contributor of inadequate vitamin D levels and activity plus low dietary calcium with impaired absorption rates. The results surprised them. While of course dietary calcium was usually lower, the Calcium absorption rate often was elevated and hormone vitamin D activity was also higher. The results did not make much sense according to expected calcium and vitamin D theories currently viewed as facts. Other mechanisms must be at work to counter these expectations. Giving extra vitamin D did not increase calcium absorption rate.
It is now known that many cell types in the body have an attachment dock for vitamin D. Here is where a dilemma surfaces. Can both the passive D and the high active hormone forms attach to these docks? Vital point # 1. ref This is still in question by some scientists. The influence of the hormone D form is 1000 times stronger than the passive D and may be due to the 1000 times stronger attraction of VDR for the active hormone D form. Vital point #2. These docks, VDR (Vitamin D Receptors) when stimulated cause the cell to create proteins that serve vital functions, such as immune activity to destroy invading disease causing bacteria. It is from the action of these proteins that many disease states are influenced by hormone D. Thus, the excitement is justified since bone health is also strengthened by hormone D increasing dietary calcium absorption. BUT, yes there might be some "buts" to deal with, read on.
NOTE: Information to clarify this passive D action now exists. Science has found at least 10 tissue cells that are capable of using the passive D form, 25(OH)D3, directly with the help of an enzyme to build the hormone D form right in these cells. Usually this hormone D does not leave the cell or tissue where it was created, but under certain conditions it does enter blood plasma with responsibility for an increased calcium blood level effect observed in specific diseases. This aspect is very new and without much clarification at this time. Of prime consideration in cells for active D production is the amount of the ENZYME, 1 alpha hydroxylase, necessary for this conversion...
When scientists compare disease rates testing the passive D levels, generally people with higher levels of passive D tend to have lower disease rates, but not always. Remember this is mostly from observational studies and the levels of D are those generated from sun exposure plus the amount from fortified foods, such as milk. In real numbers this might only be talking about blood levels of the passive D pool as high as 20-25 ng/ml versus low levels at 10-15 ng/ml. Not a very large swing in amounts. Ng/ml levels can go as high as 6o+ from sunshine production. Rarely were these early studies referring to the high levels from supplements that are now available in dosages of 2500, 5000 and even 10,000 IUs.
 Research has discovered that taking the recommended amount of 400 IUs, while it will stabilize levels, it is not enough to increase the passive D levels very much. It did prevent rickets in early studies, but may not be enough to reach levels scientists think is protective against certain cancers, autoimmune diseases, or depression, at least not without some serious sunshine exposure. (photo by Edwin Abedi)
Research has discovered that taking the recommended amount of 400 IUs, while it will stabilize levels, it is not enough to increase the passive D levels very much. It did prevent rickets in early studies, but may not be enough to reach levels scientists think is protective against certain cancers, autoimmune diseases, or depression, at least not without some serious sunshine exposure. (photo by Edwin Abedi)
- OK, now what dosages are appropriate to take? And is there an ideal level for ng/ml numbers?
These are the vital questions. But before answering them, you have to understand another important fact just recently discovered. It had been assumed that the active D form did all the work and the passive form was thought of as inert, just used as storage D material needed to build the hormone form. New research has now shown that this is not the case. More in a moment.
Another point to consider. In the blood, vitamin D binding proteins are used to ferry around the two forms of D. But, the passive form has a 1000 times greater attraction to bind with these protein carriers than the hormone form. Can you see how too much passive D could hinder the movement of the hormone form when it's actions are needed? Optimal Vitamin D Level - New Vitamin D Basics - Vitaminworkshop.com
It is known that taking 1700 IUs of vitamin D will increase ng/mL levels by about 12-15 points. Say if you start at 20 ng/mL, you would climb to 32-35. This takes about 3 months and then that level plateaus. Taking 5000 IUs could increase levels by about 30-40 ng points. It is important to know your starting amount before consuming these mega dosages so an accurate intake dosage can be determined to arrive at healthy levels, about 25-35 ng/mL. More research needs to firmly establish the most optimal level and the dynamics in influencing the hormone form levels.
SIDEBAR: There are many cases where all the signs point to what should be the maintenance of adequate passive D levels, but the readings reveal a deficiency. Scientists now know that 3 or 4 genes are responsible for the production of enzymes needed to convert the modified into pre-vitamin D cholesterol by sunshine into the passive D form (25-OHD3) in the Liver and later into the active hormone D form in the Kidneys. Thus, genetic differences account for about 50% of the variability in vitamin D levels while only 25% are for seasons and latitude (sun strength) and D intake. This explains the many non-common sense exceptions to the different seasons and latitude theory. --
The hormone D form is built mostly in the kidneys from the passive D material according to body needs. Sun exposure, fortified vitamin D foods, and supplements add to the level of the passive D pool but do not directly influence the active hormone D production. Vital point # 3. BUT, what is now also known is that at adequate levels (between 25-40 ng/mL), the passive D enters cells such as prostate, breast, and colon, and with the help of an enzyme, 1-alpha hydroxylase, can be converted into the hormone D form and directly helps protect those cells against DNA damage, mutations that could create cancer cells. Or the passive form might serve as a stage setter for the active form to perform. Both actions necessary for the active form to work. Thus, this synergistic action between the two vitamin D forms achieves the greatest effectiveness for both forms within a limited window of the passive D levels, the D factor under most direct control.
While early vitamin D studies hinted at an association to lower cancer rates, recent results have not supported a consistent cancer link except for 2 areas. First, a lower colon cancer risk from moderate D levels, 20-30 ng/mL without further influence at higher amounts, and second, a slight reduction in just the aggressive form of prostate cancer but not the non-aggressive cancers. While many breast cancer articles talk as if the link is firmly established, research has inconsistencies that warrant further study.
- Wow! I have not heard of these actions before. So you are saying that people taking vitamin D supplements, which increases the passive D levels, does not directly influence the high active hormone D production. And that the hormone form exhibits most of the influence on diseases. What does influence the production of the active hormone D?
Yes, that is mostly correct, but there are still far to many exceptions to make any rule. You cannot quickly get a benefit of hormone active vitamin D by taking supplements. An interesting sideline is that researchers often mention that as the passive D levels increase, so too does the active form with resulting greater immune protection. A study recently found that this is not necessarily always true. In fact, at very low passive D levels, higher active D levels were found 85% of the time, probably due to hyperparathyroidism. This result tips the scales of past assumptions and needs further research.
The level of calcium in the blood is the prime controller for the production of hormone D. Vital point #4. If blood calcium drops, either from low dietary calcium intake or from too much leaving the body, the Parathyroid gland secretes PTH (a hormone) to cause the Kidneys to produce hormone D. Hormone D then increases the percentage of calcium that is absorbed from foods, prevents calcium loss out of the body from kidneys and colon, and also PTH starts dissolving bones to take calcium out of bone storage until the blood calcium levels are back in balance at 1%. This 1% level is required for proper nerve, enzyme, and muscle action.
If blood calcium gets too high, the thyroid gland secretes another hormone, calcitonin, to lower PTH activity, slow down hormone D production, get the bones to store more calcium, and reduce the absorption of calcium from foods while also increasing kidney and colon channels of elimination.
NOTE: These are the true factors in calcium absorption percentages. Marketing for calcium supplements that stress increased absorption for their product are only talking about a small part of the calcium absorption story. Most calcium absorption percentages are within 5% points of each other in pure absorption tests. The real absorption % varies according to blood calcium level balance influencing hormones.
- Sounds like blood calcium balance is the real factor in deciding if bone density is increased or reduced. Have scientists tried controlling these involved hormones you just mentioned to protect against bone loss?
Yes, but just one, the intermittent use of PTH has shown the most promise, Vital point # 5, while calcitonin and hormone vitamin D (calcitriol) as well as consistent PTH have all exhibited adverse side effects. ref These truths reveal how complex the calcium balance mechanism is, and that the obvious facts, which common sense says should correct the situation, do not always work. Now let's get back to passive vitamin D pool levels and the proper level to supplement.
Usually science measures the size of the passive D pool in the blood to also reflect the (potential) active hormone D level as well. But remember, the 2 vitamin D pools are not always related, and that past assumptions as to how they should behave may not in fact be the reality. It is possible to have low passive levels and high active, or just the opposite. Vital Point # 6. The passive D pool cannot reach a toxic level from just sun exposure while it can from supplemental vitamin D. There is a failsafe feedback loop that stops overproduction of sunshine D or prevents it from increasing the passive D pool beyond certain limits. Vital point # 7. This feedback is actually also generated from sunshine exposure. **also look for VBP at bottom**.
- There are nutritionists that say the body makes thousands of vitamin D units from less than an hour in the sun. Your Vital point #7 appears to contradict that message. What's the story?
The scientists that first measured this amount did not have all the facts currently available to reach the true influence. Nutritionists since then have just parroted these results and not logically put the facts together. It just doesn't happen that way. The body probably does produce thousands, but just as quickly much of it is neutralized by a feedback loop and either eliminated or put into fat storage for later lean sunshine times. It does not all get into the body to increase the passive D pool levels beyond nature's safe level (maxing out at about 60 ng/mL or 150 nmol/L). Sunshine produces the elements that participate in this feedback loop. BUT they are not produced when taking supplements. ref See surfer chart below. (These effects may develop overtime)
- That is a novel concept that really should impact supplement discussions. Now are you ready to link the vital points together and tell how much "D" is safe to take?
Yes, the answer to "what is the best level to take?" is the amount that gets the body to the safest and most effective passive D pool level, about 25-35 ng/ml (65-90 nmol/L). If you are now at 10 ng, you could take 2500 IUs for about 3 months and measure again at that time. Researchers say it takes about 100 IUs to raise the ng/ml level by about 1. From 10 to 35 you need to raise by 25 units times 100 = 2500 IUs. When you arrive at the 35 ng/ml level, it is still open as to how much D you need to take to maintain that level. Maybe 400-1000 IUs would hold. It is always wise to take higher levels in the winter when less sunshine. Plus, one could always just use the higher amounts in the winter and not take D or at very low amounts in summer. Remember, some sunshine is also necessary for the extra elements for complete D function. This just might be the safe route until long term results settle these issues.
The following is an excerpt from www.medscape.com/viewarticle/589256_8 "How much vitamin D is needed per day to obtain a normal vitamin D blood level? The following examples include:
- 400 IU (10 mcg) per day increases vitamin D blood levels 4 ng/ml (10 nmol/L).
- 800 IU (20 mcg) per day increases vitamin D blood levels 8 ng/ml (20 nmol/L).
- 1000 IU (25 mcg) per day increases vitamin D blood levels 10 ng/ml (25 nmol/L).
- 2000 IU (50 mcg) per day increases vitamin D blood levels 20 ng/ml (50 nmol/L).
If the vitamin D blood test was 20 ng/ml (50 nmol/L) and a 40 ng/ml (100 nmol/L) level was desired, 2,000 IU (50 mcg) of vitamin D per day over several months should be taken to achieve a normal blood level or 40 ng/ml (100 nmol/L). Upon reaching the goal, most individuals need to supplement with 800 to 1,000 IU per day to maintain this level. Only working closely with a clinician over time can provide the most accurate answer. However, issues of insurance and health care access suggest that 800 to 1,000 IU is ample for many individuals who are not able to have their blood tested."
Amounts will vary slightly from person to person, sun exposure, D from diet, calcium and other minerals that influence calcium levels (sodium, potassium, magnesium, and phosphorus) amount of protein in diet, caffeine. and exercise. NOTE: Research shows it takes 1500 IUs to maintain this level over winter for Seniors without any sun exposure or fortified foods. This amount is reduced with sun exposure time and consumption of fortified foods. Thus, a supplement amount of 1000 IU may be pretty close.
- There is another number that some nutritionists use to measure D levels that is higher than the ng/mL amount. How do the numbers relate?
Yes, the lower numbers are for ng/ml, nanograms per milliliter while the higher numbers are for nmol/L, nanomoles per liter. They measure the same thing. To convert ng to nmol, multiply by 2.5 (30 ng/ml = 75 nmol/L)
- Now, since these amounts are somewhat lower than Dr Mercola and some nutritionists are recommending, what happens if you continually take high vitamin D amounts? Does the passive D pool level keep increasing?
Glad you asked that. This is the question that without longer term studies, no one is really too sure yet. It appears that a given amount of vitamin D units will only raise passive D levels to a certain level and not beyond. There have been some speculations. This is where I go into my possibility theories and tie up the vital points. I want to start by showing a couple of charts that point to some interesting associations.
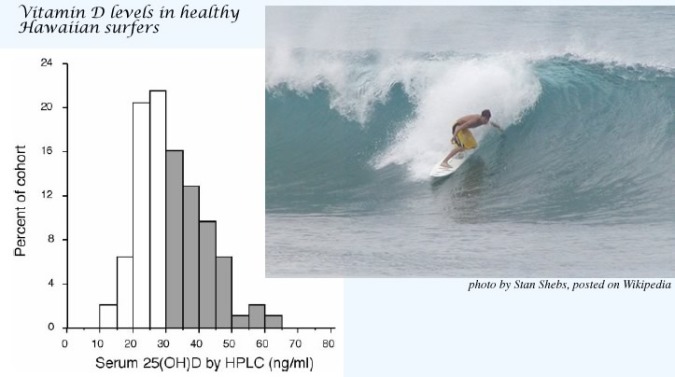
Surfers in Hawaii from lots of sunshine exhibit an average passive D level of just over 30 ng/ml. If the sun produced 10,000 units every day, they would have much higher levels. With only 10% of surfers reaching levels of 55 to 65 ng/mL, this reveals the protective feedback loop the body uses to not let the passive pool go too high. Nature may have a reason for this. The skin darkening from the tanning effect also limits future sunshine D production. Plus, not sure if any of them were taking any supplements or how much fortified foods they were consuming which may have elevated some amounts. ref
PRIORITY NOTE: The information given out that supplemental vitamin D at 10,000 IUs is safe because 15-20 minutes of full sun exposure generates about the same as 10,000+ IUs is flawed. Hollis, Heaney, Hollick*, Veith, and other vitamin D experts should know better than to allow this to stand uncontested. The way this level was determined reveals the error. A tanning bed light was used for 20 minutes to generate 1 MED which is the point at which sunburn starts to mimic sun exposure and the increase in vitamin D as 25 OHD was measured in the blood. A supplement of vitamin D2 was given at 10,000 IUs and found to reach the same 25 OHD blood amount. Thus the 10,000 must be safe level. The error is that it is now known that over time and at higher doses, vitamin D2 is only about 33% (anywhere from 10 to 50%ranges considering individual variations) as effective as vitamin D3, thus this really is only about 3300 IUs of supplemental vitamin D3 and not 10,000 IUs, the level of many new vitamin D3 supplements. ref Plus, the protective feedback process that is also initiated by sunshine that prevents or stops any excess passive D buildup is bypassed when supplemental vitamin D is consumed. It is possible this tanning bed study may have stopped before the feedback loop went into effect. Vitamin D2 may only be 30% as effective due to its rapid clearance out of the body compared to D3 which has a much longer lasting influence. Thus, while short term effects are similar, longer term are not. And there could potentially be metabolic differences that are more subtle at lower doses.--- D3 vs D2, note only 11 week study> ref ref
*Dr. Hollick at least is cautious about mega-dose D supplements and recommends sensible sunshine exposure with moderate supplements to increase D levels. He is researching the vitamin D control elements produced by sunshine to discover their function and relationship to controlling the overall level. The above study on D2 vs D3 was only for 11 weeks. D2 reduced D3 level, while overall total remained the same. Long term result of this change is not yet known.
CAUTIONARY NOTE: It is now known that a genetic change to genes influencing vitamin D receptor activity may be associated with calcification of arteries, a condition leading to heart disease. From animal and some human studies, people exhibiting this B allele modification had higher amounts of calcium deposited, especially tested for in the aortic heart valve. For this group, both low levels plus taking higher amounts of vitamin D might put them at jeopardy for accelerating this disease process by increasing calcium blood levels or changing calcium/ magnesium/ phosphate balances as influenced and highlighted in Kidney disease.--
OF INTEREST: The hormone form of vitamin D influences arterial calcification. A high hormone D level is associated with less calcification of arteries. Vitamin K2 is a vital factor here too.
The next chart shows in the shaded area with a line down the middle for averages, the associations between the plotted mortality (death) rates at each passive vitamin D level. This information is from a large study over many years (NHANES). The lowest point with the fewest deaths is also at about 35 ng/ml. Above that amount, the top shaded area starts to increase. Yes a very few do go a little bit lower, but it is the increasing death rate part on top over 35 ng/mL that is of most concern. The scientific explanation for this increase is still missing from most vitamin D discussions. These two charts lead me to believe that it may not be wise to go any higher than 45 ng/ml, or any lower than 25 ng/ml. Do you agree with my analysis?
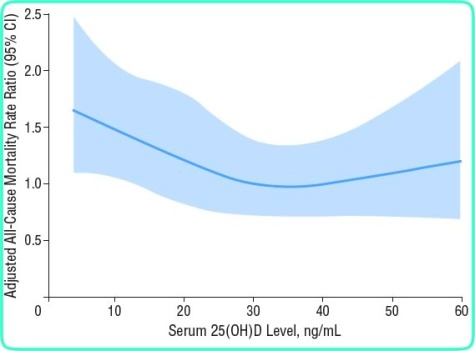
- I see what you mean and yes, I do agree. It is very disconcerting that nutritionists are going overboard on dosages without much long term research. I read on the Vitamin D Council's website they recommend 50 - 80 ng/mL levels. Now, are there any possible explanations for these observed mortality associations? And are there any other long term effects from these mega dosage vitamin D supplements?
***Please study the info on this reference Same as above for surfer study. Notice the Hip fracture rates at various D levels. Play with the D Metabolism animation. Vitamin D appears to have risks at both low and high amounts. Not many if any Nutritionists are telling you the complete Vitamin D story. Also the cancer links are all over vitamin D levels, such as increased Prostate cancer risk at normal to medium high levels. ref <VERY IMPORTANT LINK to show how vitamin D might influence aggressive PROSTATE CANCER risk by increasing INSULIN.
POSSIBLE ADVERSE EFFECTS OF HIGHER D AMOUNTS
First, there are some adverse effects that need to be addressed, even though some are quite infrequent. Higher D levels have exhibited increased renal (Kidney) disease, an important consideration for breast cancer survivors, increased calcium blood levels, and increased gastrointestinal symptoms, and most troubling, a doubling of the pancreatic cancer rates was found in people exhibiting the highest vitamin D levels versus those at lower levels, at least in one study. ref A new meta-analysis study found the opposite that vitamin D protects against pancreatic cancer. ref Plus a long term association is just beginning to emerge that autoimmune conditions might be connected at both ends, deficiency and excess, but more research is needed to discover mechanisms.
A recent report on Fragility in Seniors found the most protective levels of passive D were between 20 - 29 ng/mL. http://www.medpagetoday.com/Geriatrics/GeneralGeriatrics/23810 In this study, both 15 and 30ng/mL showed about the same degree of fragility adverse effects. The fragility factors included 3 of the following; weight loss, weakness, exhaustion, slowness, and low physical activity. Below 15 ng/mL, 47% increase in factors while 32% over 29.9 ng/mL.
While not enough long term research exists, there are a few theories that could explain possible functions of increasing passive D levels. If both the passive and the hormone D forms can attach to cell VDR docks. The reason that the hormone D form has a 1000 greater VDR activity compared to passive D could be due to the fact that it exhibits a 1000 times stronger attraction to VDR docking sites. If this is true, as the passive D pool continues to increase from these megadose vitamin D supplements, it could reach a point where it starts to bind up too many Vitamin D receptors which would limit the 1000 times stronger hormonal D activity from binding to VDR when needed. UPDATE: check out article on Vitamin D Binding Protein, DBP
Just ten years ago it was discovered that in some tissues such as prostate, breast, and colon, the vitamin D converting enzyme changes the passive D form into the hormonal D right in the tissue cells. This directly protects these tissues. At the passive D deficiency levels common today, especially from the campaign to limit skin cancers, the levels may be too low to adequately perform this function. This would leave these 11 tissues more vulnerable to disease initiation.
There may be an opportune range or window of passive D amounts that if exceeded would change dynamics from protective to adverse effects. The end result is that as the body tries to maintain the proper body vitamin D receptor functions, it is not known at what levels of the two types of vitamin D's this adaptation starts to either kick in or starts to fail. This might explain the mortality increases at both low and higher amounts on the above chart. The body wants to maintain balance and harmony from self regulation. Why does the body set limits on the generation of sun produced vitamin D3 and control the passive D pool size? reference The optimum passive D level is simply not completely known yet and may very well be different for certain subsets of individuals or at different ages, such as for those with the D allele modification. ref
NOTES: At least 3 different amounts are often mentioned as most beneficial for three areas of D actions. Lower at around 25 ng/mL for bones, 35-40 for immune system, and 40+ for cancer prevention. And here should also be noted that higher vitamin D levels also can increase toxic heavy metal absorption such as lead along with the essential minerals, calcium, magensium, phosphate, zinc, selenium, iron.
This concept of pool size interference is also seen in digestion when minerals and vitamins compete for the same docking sites or carrier transport proteins. i.e. Calcium to magnesium, zinc to copper, vitamin E to vitamin K. There may also be an issue with plasma protein carriers in arteries between the different vitamin D forms as well. As the passive D pool increases, this form could bind up more protein carriers and thus limit the active D form transport capabilities. So far, this appears to only be a factor in disease states of the liver and kidneys and not for healthy people. Vitamin D Binding Proteins (DBP) are usually very abundant.
There is some science to support that one of these processes is indeed what is happening, or maybe a little of both. Watch for updates. It is difficult to measure these effects in the body. But the one fact that is known and not a theory, hypercalcemia, or high calcium induced by high vitamin D intake, does come into play with supplements but not from natural sunshine produced vitamin D3. The body has numerous natural feedback loops to limit vitamin D metabolite levels. Supplements bypass many of these mechanisms.
NOTE: Research now shows vitamin D3 circulating levels as 25-OHD are capable of increasing calcium absorption without increasing 1,25OH2D, the hormone form, at 1/8 of total calcium absorption, an amount much greater than in test tube studies. This adds another aspect for dosages of both calcium and vitamin D playing a role in calcium balance and resulting disease associations for bone health, artery health, breast and prostate, and colon. ref -end note
Now before wrapping this up, one more point needs to be addressed. And that is about the influence of high calcium supplementation on the two vitamin D form levels. Remember when it was mentioned that the various calcium regulating hormone treatments and that the only one showing promise was the intermittent use of PTH. Intermittent use means rotating on and off consumption periods. Maybe the body with its elaborate blood calcium balancing mechanisms isn't designed to function correctly either always having an excess calcium intake or at a constant low deficiency intake. At a continuously high calcium intake, the body does not need to activate the hormone D form which has as its primary function to increase calcium and phosphorus absorption. High calcium intake, low active hormone D production, low passive D pool levels, a constant either always low or always high PTH level, and you have the perfect storm for not only bone fractures, but also increased cancers, heart disease, depression, type 2 diabetes, and autoimmune conditions.
One more issue may have significance. From animal studies it was discovered that higher vitamin D intake not only increased calcium and phosphorus absorption, but also that of lead. The importance of this is of course determined by the amount of lead in the foods or supplements consumed. Health food consumers could be at a disadvantage since whole and concentrated foods often have higher lead content than processed foods, especially green foods such as cereal grasses and algaes.
- I think these concepts could be some of the most profound conditions for health. It would better explain many of the seemingly controversial findings about why there is so much confusion over the impact of vitamin research on diseases. An improper understanding about body principles, physiology, and nutrition. Would you now summarize the most important points?
The Vitamin D scene is really exploding quite rapidly. But one has to temper these early reports until longer term studies are completed. Quite a few factors are happening at the same time which might confuse and mask the real influences, such as knowing if you have the B allele modified gene factor. There appear to be two important functions for the proper passive D levels, to generate the in organ hormone D production for tumor prevention and also to produce the blood levels of hormone D needed for calcium maintenance. Science has yet to correctly determine this level.
One more fact needs to be clarified, It is important to have adequate but maybe not too much calcium to go with sufficient vitamin D, both of which are important for normal cell processes to stop cellular DNA damage, control cell divisions, and cell life spans, all critical issues to prevent cancer initiation and artery wall damage. High calcium intake may be detrimental if vitamin D levels are low, a far to common situation today. BUT, it is not necessary to take them both at the same time. The D taken with calcium will not enter the body's pool untill long after that calcium has passed the absorption point. Vitamin D levels take about 2 to 3 months to build up to the maximum level that the consumed amount will achieve.
Researchers have also discovered that higher calcium intakes can compensate for low vitamin D status for some bone health issues, This could be the information used to establish the current FDA extremely high calcium recommendations, up to 50% higher than the rest of the World. The downside is that this could increase potential risks for adverse effects from excess calcium shutting down hormonal vitamin D production.
UP to 75% of people may be deficient in vitamin D passive pool levels thanks to sun avoidance. Obesity is contributing to lower D levels as fat binds more vitamin D, plus reduced cholesterol levels also might decrease natural sun D production since it is known that low cholesterol reduces infection fighting ability and vitamin D increases it.
There are a lot of generalizations being used as facts and creating confusion over the proper course for supplement amounts. The opposite extreme risk of high vitamin D intake is not only for increasing calcium levels too much, but also as an enhancement of calcium activity. Soft tissue calcification is a vital issue. Associations are under investigation for dementia and artery disease leading to heart attacks, plus the possibility of long term bone fracture increases from replicative capacity exhaustion of bone building cells.
Most important is that sun vitamin D production has built in body limits while supplement vitamin D does not. This speaks volumes that the precautionary principle should be in play, but it is not judging by the rush to higher potency vitamin D supplements without adequate usage instructions and body level measurements.
And last, that the passive vitamin D pool size does not influence how much hormone D is produced, although much of the literature assumes this connection. In some disease states there exists a low passive D level but a very high hormone D level. There appears to be a total failure to view the complete picture of vitamin D body processes by some nutritionists. Until they figure it out, mother nature may be the best guide.
NOTE: The preceding discussion concerns nutritional levels. Some Doctors give patients vitamin D2 at much greater amounts such as 50,000 IUs, but not everyday. This is to quickly ramp up the passive D pool. Some people have lower conversion rates and it takes them longer to increase levels. Constant measuring of the passive D pool level is needed. There is still controversy over the desired passive D level and how or if it starts to interfere over a certain level. A diseased condition could lower passive D levels. Conversion to the hormone D form would use up the passive D levels. And breakdown vitamin D metabolites from both the hormonal and passive D forms also influence body functions and act as regulators. A higher D passive pool means a greater amount of metabolites would be created. Many Long term effects are still unknown at this time.--
Addendum 12-1-10: There is some evidence that high vitamin D supplementation could enhance any deficiency effects of magnesium. Magnesium and a few other nutrients such as vitamin K2 serve as vitamin D co-factors necessary for proper utilization of vitamin D processes. Just increasing magnesium levels might help support vitamin D activities. Plus, of equal significance, higher vitamin D intake could increase lead and other heavy metal absorption, depending upon the level of lead in food and supplement choices.
It's your choice which camp you follow, nature or science. But since science is still incomplete, the wise choice should be nature.
The next article contains reports copied from a Government (National Institutes of Health) sponsored Vitamin D workshop:
"In October 2003, the NIH cosponsored the Vitamin D and Health in the 21st Century: Bone and Beyond conference, which explored the role of vitamin D in osteoporosis and other diseases. Participants concluded that overall, Americans' current intakes of vitamin D may be too low for optimal health.
Copied to prevent loss of links to the vital information presented at this Vitamin D workshop. See next article below or go here for rest of D workshop...
|
Plus, here are two other website articles on this subject:
|